Artificial intelligence (AI) and machine learning are changing many industries, including healthcare. In radiology, AI is becoming more important. This raises a big question: Can AI replace radiologists in Canada?
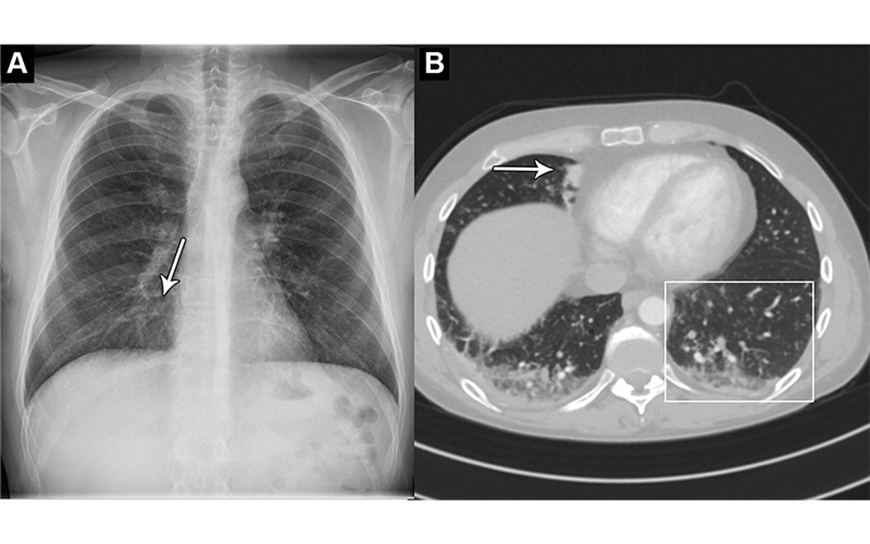
AI can now analyze medical images like X-rays and MRIs very well. This makes some worry about the future of radiologists. AI can spot small problems that humans might miss.

But, the debate about AI and radiologists is complex. AI can make some tasks easier and more accurate. Yet, radiologists bring a unique skill to patient care. It’s important to use AI wisely in radiology to help patients in Canada.
AI Radiology: The Potential and Limitations
AI in radiology is very promising. It can make medical imaging analysis more accurate and efficient. This means radiologists can do less repetitive work and focus on harder cases.
But, there are also challenges with AI in medical imaging. AI needs lots of good data to work well. Getting this data is hard, especially because keeping patient information safe is very important.
AI can also show biases if the data it’s trained on is biased. This can lead to wrong diagnoses. We need to make sure AI is fair and works for everyone.
Adding AI to how radiologists work is also tricky. It needs to fit smoothly into their daily tasks. This requires careful planning and making sure everyone trusts and uses the technology.
The Potential of AI in Radiology
- Improved accuracy and efficiency in medical image analysis
- Automated detection of subtle patterns and abnormalities
- Expedited diagnoses and reduced workloads for radiologists
Limitations and Challenges of AI Adoption
- Requirement for large, diverse, and high-quality datasets
- Potential for algorithmic bias and skewed results
- Seamless integration into existing radiology workflows
| Potential of AI in Radiology | Limitations of AI in Medical Imaging |
| Improved accuracy and efficiency | Requirement for large, diverse datasets |
| Automated detection of abnormalities | Potential for algorithmic bias |
| Reduced workload for radiologists | Challenges of integration into workflows |
The Human Touch: Why Radiologists Remain Invaluable
In today’s world, where AI is changing healthcare, radiologists are still key. AI has improved medical imaging, but radiologists bring something special. Their skills and understanding are crucial in the role of radiologists in AI-driven healthcare.
Clinical Expertise and Contextual Reasoning
Radiologists have a unique mix of skills. They know how to read medical images well, thanks to their training and experience. They can spot things AI can’t, making accurate diagnoses.
They use patient history and symptoms to understand medical images better. This importance of human expertise in radiology leads to more accurate and personal interpretations. These are key for making the right treatment plans and improving patient care.
Radiologists also know a lot about human bodies and medical imaging. They can spot and fix problems in AI’s work. Their knowledge is a safety net in the world of AI healthcare.

Even as AI changes healthcare, radiologists are still essential. Their human touch and expertise are vital for accurate and relevant medical imaging. This benefits patients and improves healthcare quality.
Integrating AI into Radiology Workflows
The medical world is now using artificial intelligence (AI) in radiology. The big challenge is to fit these new tools into our current work flows. It’s all about working well with AI, making sure it’s right, and using it wisely.
It’s key for radiologists and AI makers to work together. They can use their skills to solve healthcare’s big problems. Radiologists know the clinical side, and AI experts can make the tech better and easier to use.
Testing and checking AI tools is also very important. They need to be checked to see if they work well and fit with what we already have. This makes sure AI is safe and works right in radiology.
Following the best ways to use AI is also crucial. This means setting up clear rules, having good leadership, and training everyone. This way, we can get the most out of AI without any problems.
By working together, testing well, and following the best practices, we can make AI in radiology better. This will help us care for patients better, work more efficiently, and keep improving our field.
Ethical Considerations and Challenges
AI is changing radiology fast, but we must face the ethical issues it brings. We need to look at data privacy and algorithmic bias in AI radiology.
Data Privacy and Bias Concerns
The healthcare world deals with very private patient data, like medical images. With AI, there’s worry about keeping this data safe. We need strong rules and ethics to use AI right in radiology, keeping patient info safe.
There’s also a big worry about AI bias. AI learns from old data, which might show biases. If we don’t fix this, AI could make unfair or wrong diagnoses, hurting some patients more. It’s key to make AI fair and inclusive for everyone’s health.
| Ethical Concern | Description |
| Data Privacy | Protecting patient confidentiality and preventing unauthorized access to sensitive medical data |
| Algorithmic Bias | Addressing the risk of biased AI algorithms that can lead to inaccurate or discriminatory diagnoses |
Fixing these issues needs teamwork from doctors, AI experts, lawmakers, and patient groups. With good rules and ethics, we can use AI in radiology right. This will help patients and keep everyone’s health safe.
Conclusion
The future of radiology is closely tied to AI and machine learning. These technologies are changing the field, making it more efficient and accurate. But, radiologists are still key, bringing their expertise and understanding to patient care.
Working together, radiologists and AI can make a big difference. They can improve how images are read and make decisions better. But, it’s important to think about ethics, like keeping patient data safe and avoiding AI biases.
Radiologists will be crucial in the future of healthcare. They can use AI to help, but still keep the human touch important. This way, they can make healthcare better for everyone, making it more efficient and fair.
FAQ
What is the impact of AI on the field of radiology?
Artificial intelligence (AI) is changing radiology a lot. It could make diagnoses more accurate and work more efficiently. AI tools help with image analysis and finding diseases, changing how radiologists work.
What are the potential benefits of AI in radiology?
AI could make image analysis better and faster. It might also help radiologists by finding things they miss. AI can also help sort cases, so radiologists focus on the most important ones.
What are the limitations and challenges of AI in medical imaging?
AI has a lot of potential but also faces challenges. It needs lots of data and can be biased. It’s also hard to fit AI into current healthcare systems. Working together is key to solving these problems.
How can radiologists and AI work together effectively?
Radiologists and AI developers need to work together well. This means testing AI, following best practices, and setting rules for using AI. This ensures AI is used responsibly in medicine.
What are the key ethical considerations in the use of AI in radiology?
Using AI in radiology raises big ethical questions. There are concerns about privacy and bias. We need strong rules and guidelines to use AI fairly and safely in medicine.


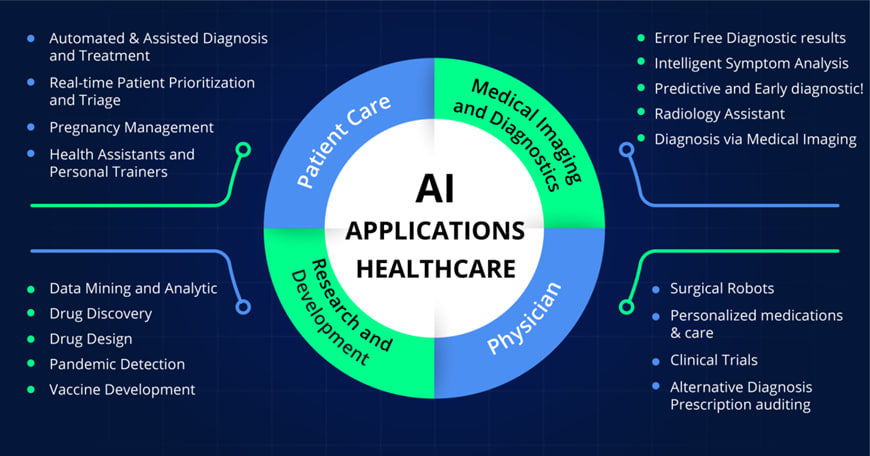 Artificial Intelligence (AI) has revolutionized predictive analytics in patient care, offering new opportunities for early diagnosis and personalized treatment. This proactive approach marks a significant shift from the traditional reactive stance of clinicians.
Artificial Intelligence (AI) has revolutionized predictive analytics in patient care, offering new opportunities for early diagnosis and personalized treatment. This proactive approach marks a significant shift from the traditional reactive stance of clinicians.