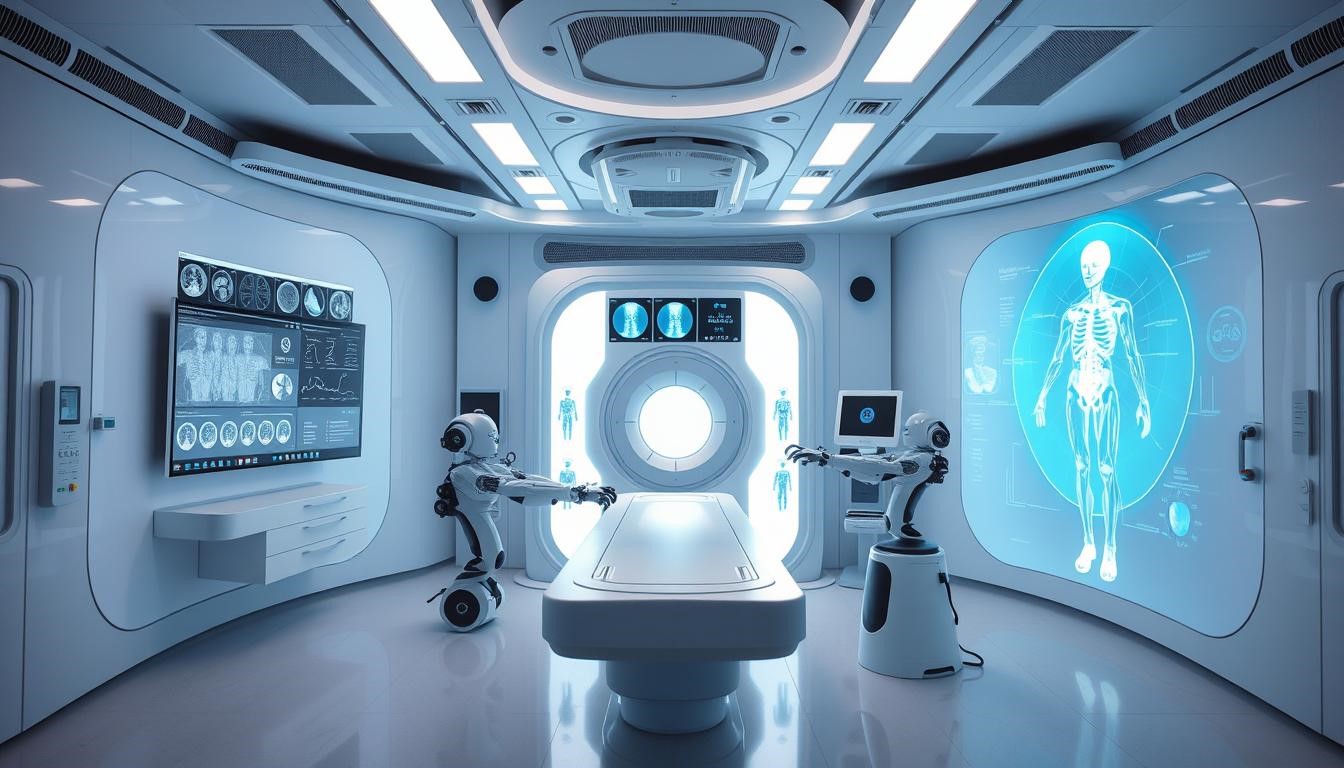
AI in healthcare is changing how doctors find diseases early. Medical imaging technology is key to this change. It lets doctors spot health problems before they get worse. This way, they can act quickly to prevent serious issues.
Spotting diseases early is essential for better patient care. AI in medical imaging is a big help here. It looks through lots of medical data to find signs of disease. This lets doctors act fast, lowering the chance of serious problems and improving treatment results.
As medical imaging tech gets better, we’ll see more AI uses in healthcare. This will lead to even better health for Canadians.

Understanding Early Disease Detection with AI in Medical Imaging
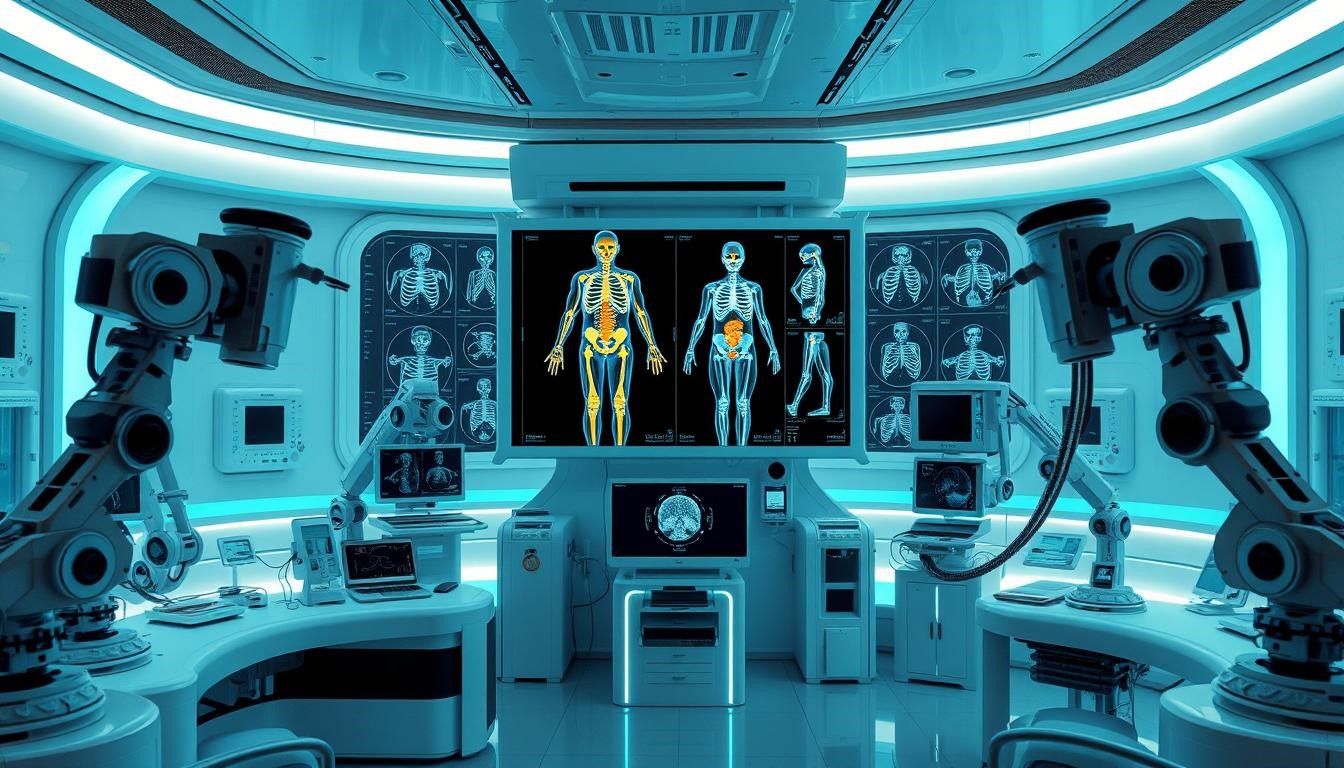
Medical imaging has changed a lot over the years. This change is thanks to new technology and healthcare innovation. Now, AI helps doctors find diseases early. Let’s look at how AI in medical imaging works, its benefits, and what makes it special.
The medical imaging evolution is amazing. It has moved from old methods to using AI today. AI makes doctors better at spotting diseases by looking at images more closely and fast. It uses machine learning to find patterns and problems in images, helping find diseases early.
- Machine learning algorithms for image analysis
- Data storage and management for efficient image retrieval
- User-friendly interfaces for healthcare professionals to interact with AI systems
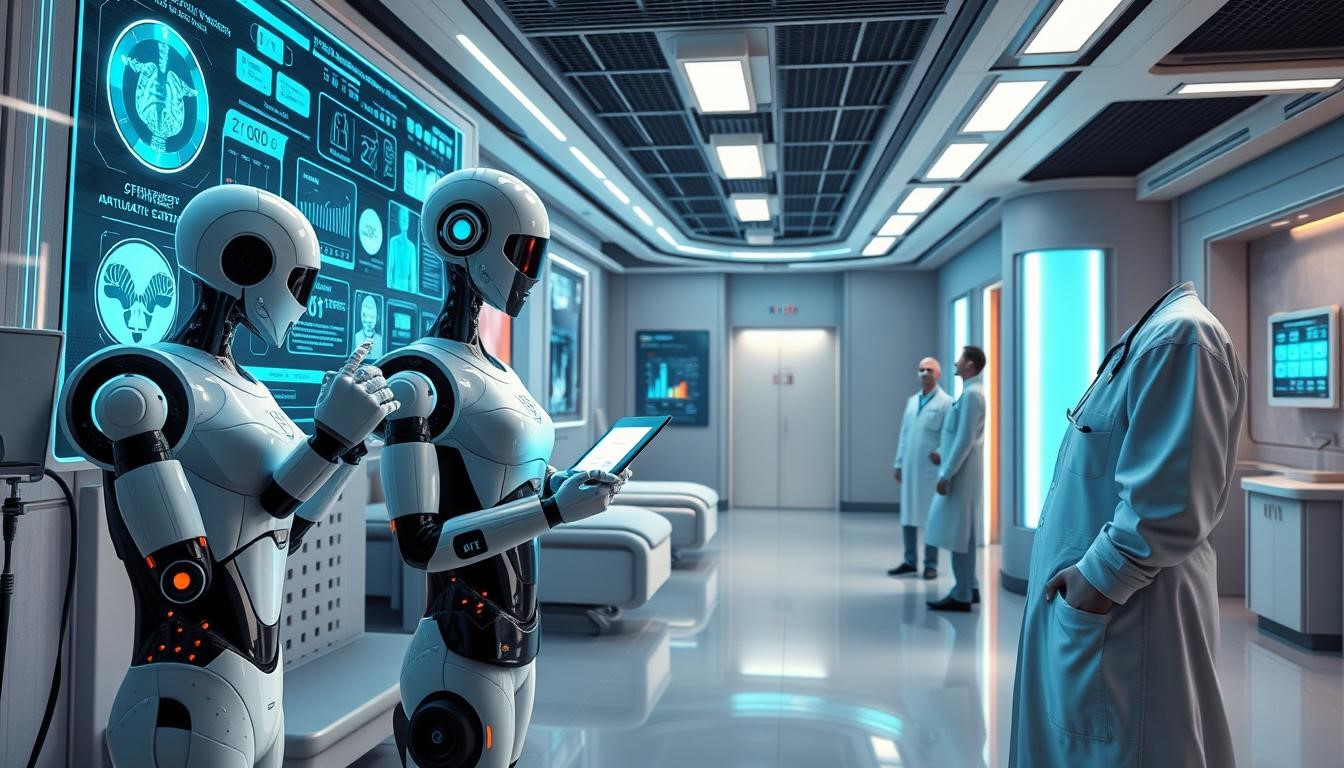
Using AI-powered diagnostic tools helps doctors do better work. It makes patients healthier, saves money, and improves care quality. As healthcare innovation keeps getting better, we’ll see even more advanced AI in medical imaging. This will change how we find and treat diseases.
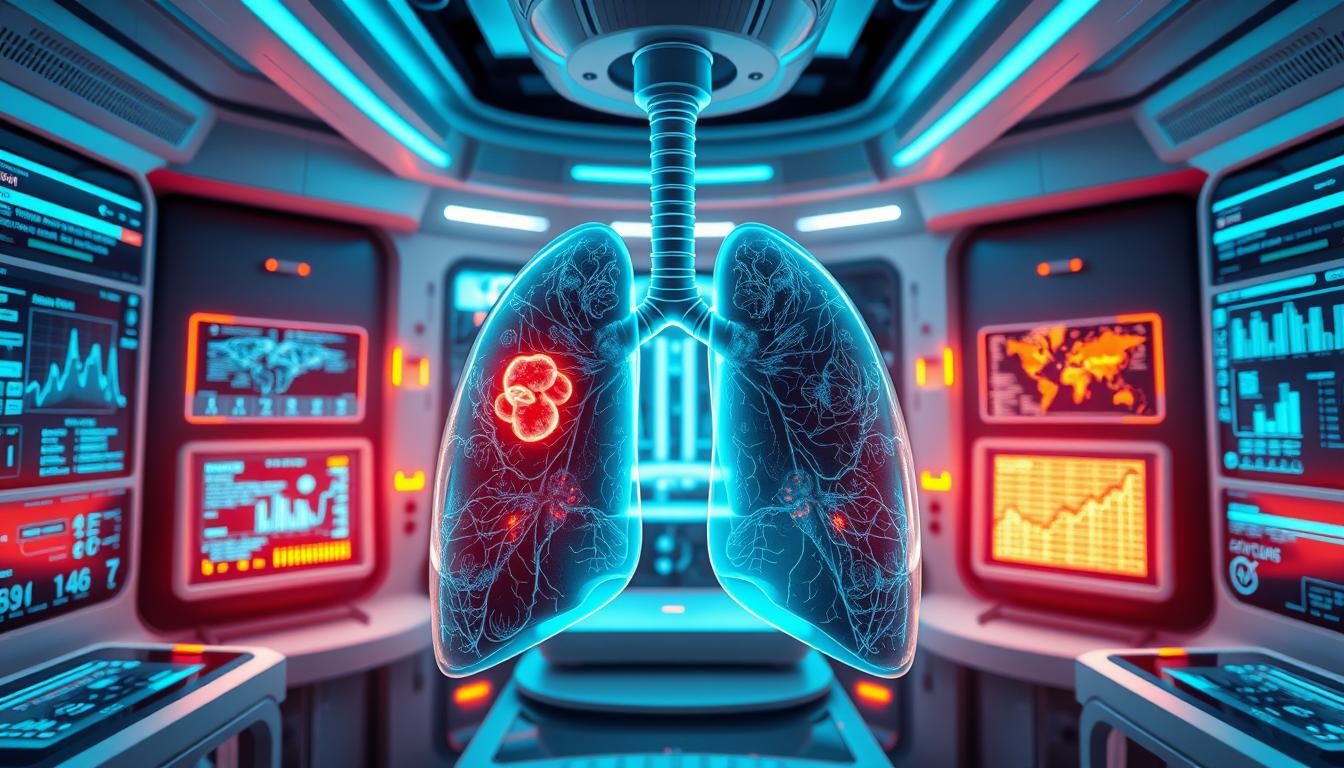
Revolutionary Applications in Different Medical Fields
AI in healthcare is changing the medical world. It brings new ways to care for patients. For example, AI helps find tumors faster and more accurately. This means doctors can start treatments sooner.
In cardiology, AI looks at medical images and patient data to spot heart disease. This new tech could change how doctors diagnose and treat diseases. AI helps doctors give care that’s more tailored to each patient, leading to better health results.
- Enhanced diagnostic accuracy
- Personalized treatment plans
- Streamlined clinical workflows
These changes are making healthcare better and more proactive. As AI grows, we’ll see even more ways it can help in medicine. This will lead to better care and health outcomes for everyone.
Benefits and Implications for Canadian Healthcare
AI is changing Canadian healthcare in big ways. It helps find diseases early, making healthcare better and cheaper. This is especially good for rural areas where getting to a doctor can be hard.
Some big benefits of AI in healthcare include:
- Improved diagnostic accuracy and speed
- Enhanced patient care and outcomes
- Increased cost-effectiveness and resource optimization
- Expanded rural healthcare access through remote diagnostic capabilities and specialist consultations

Studies show AI can save a lot of money for healthcare. It makes sure resources are used well and cuts down on unnecessary tests. This helps ease the financial stress on healthcare. AI also helps rural areas get better care and tests without having to travel far.
AI is making a big difference in Canadian healthcare. It makes diagnoses better, care more effective, and saves money. As healthcare in Canada keeps changing, AI will likely play a bigger role. This includes making healthcare better in rural areas and saving money.
Overcoming Implementation Challenges and Safety Considerations
AI tools are becoming more common in healthcare. It’s key to tackle the challenges and safety issues they bring. One big problem is data privacy. It’s vital to protect patient info. Healthcare groups must have strong security to keep data safe and follow the law.
Another important point is training requirements for healthcare workers. They need to learn about AI systems and how to use them. This includes knowing what AI can do and its limits, and the rules for using it.
- Make and follow strict data privacy rules and steps
- Offer detailed training for healthcare staff on AI and its use
- Set clear rules for following AI rules and standards
By dealing with these issues, healthcare places can use AI tools well. This will help patients get better care and improve the quality of care overall.
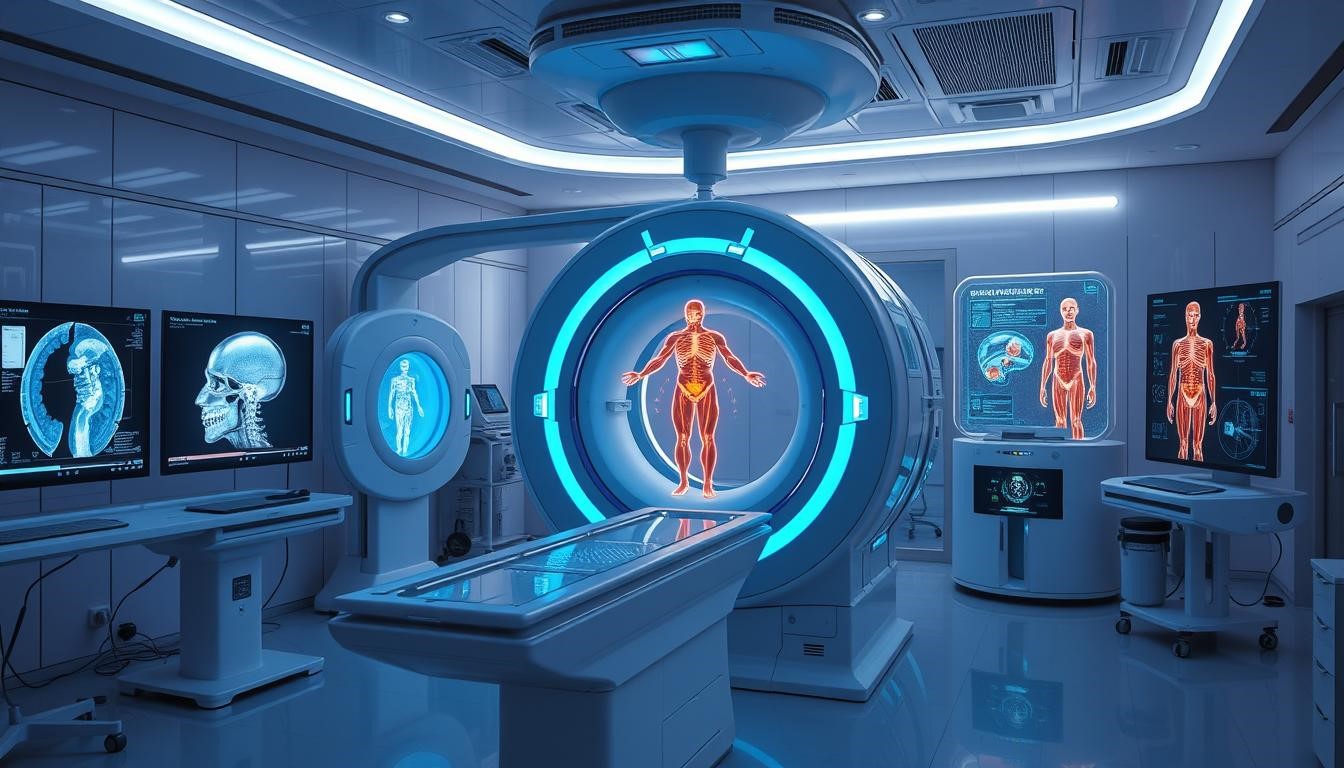
Conclusion: The Future of AI-Driven Disease Detection
AI is changing healthcare in big ways. It’s making care more personal, proactive, and effective. By combining advanced medical imaging with AI, we’re getting better at finding diseases early.
This change is making healthcare better at stopping and managing many diseases. We’re looking forward to AI getting even smarter. It will spot tiny changes in medical images, helping us catch diseases early.
AI will also work with the Internet of Medical Things (IoMT). This means constant monitoring and analysis of health data. It will help doctors give care that fits each patient’s needs.
AI is making Canadian healthcare more accurate and efficient. It will help people in rural areas get better care. And it will lead to better health for everyone. With AI, healthcare is becoming brighter, more efficient, and focused on keeping people healthy.
FAQ
What is the role of AI in early disease detection through medical imaging?
AI is changing how we find diseases early. It makes medical image analysis faster and more accurate. AI uses advanced algorithms to spot small changes in scans, helping doctors diagnose quicker and more precisely.
How does AI improve diagnostic accuracy in medical imaging?
AI algorithms are super precise in analyzing medical images. They catch tiny changes or anomalies that humans might miss. This means diseases can be found earlier, leading to better treatment options.
What are the key components of AI-powered imaging systems?
AI imaging systems have a few main parts. These include machine learning algorithms, lots of data, strong computers, and easy-to-use interfaces. Together, they help analyze images, offer insights, and guide doctors in making decisions.
How can AI be integrated into Canadian healthcare systems?
AI can be added to Canadian healthcare in several ways. It can make diagnosis faster, use resources better, and help people in remote areas get care. This makes healthcare more efficient and cost-effective.
What are the challenges and safety considerations in implementing AI for early disease detection?
There are a few big challenges. Keeping patient data safe, training doctors on AI, and following rules are all important. Solving these issues is key to using AI safely and ethically in healthcare.
What is the future outlook for AI-driven disease detection?
The future of AI in disease detection looks bright. We can expect better algorithms, more use in prevention, and AI working with new tech like the Internet of Medical Things (IoMT). This could make healthcare more proactive, personalized, and effective.