Introduction
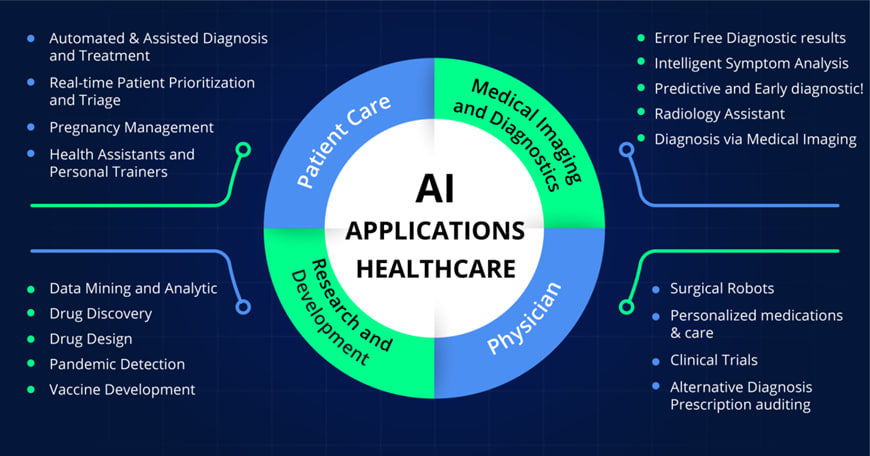
The advent of artificial intelligence (AI) is ushering in a new era in the field of healthcare, particularly in the realm of medical imaging. As the volume and complexity of diagnostic imaging continue to rise, radiology is increasingly turning to AI technologies to enhance clinical workflows and improve patient outcomes. This integration not only aids radiologists in interpreting images with greater precision but also optimizes the overall efficiency of radiological practices.
The implications of AI in radiology extend beyond mere image analysis; they encompass a wide range of applications that promise to transform patient care. This article investigates the multifaceted roles of AI in radiology, including advancements in image enhancement, automation of reporting processes, and the integration of diverse imaging modalities. Furthermore, it highlights how AI-driven predictive analytics can inform clinical decision-making, ultimately leading to more personalized and effective patient care. By exploring these innovations, readers will gain a deeper understanding of how AI is redefining the landscape of radiology and paving the way for a future characterized by improved diagnostic capabilities and enhanced healthcare delivery.
Predictive Analytics in Patient Care
 Artificial Intelligence (AI) has revolutionized predictive analytics in patient care, offering new opportunities for early diagnosis and personalized treatment. This proactive approach marks a significant shift from the traditional reactive stance of clinicians.
Artificial Intelligence (AI) has revolutionized predictive analytics in patient care, offering new opportunities for early diagnosis and personalized treatment. This proactive approach marks a significant shift from the traditional reactive stance of clinicians.
Risk Assessment Models
Recent advances in imaging technology and AI, particularly deep learning-based risk models, show great promise in improving the accuracy of personalized risk assessment. Multiple studies have demonstrated that factors such as high breast density, complex mammographic tissue patterns, and marked background parenchymal enhancement on MRI scans are linked with increased lifetime risk for breast cancer.
AI-based models use imaging data to predict short-term risk by detecting early signs of breast cancer invisible to the human eye. One recently developed mammography-based deep learning algorithm, Mirai, accurately estimates the 1- to 5-year risk of breast cancer across diverse patient populations, outperforming many existing clinical risk models . In an externally validated study, it demonstrated better 1-year risk prediction than 3-year risk prediction (area under the receiver operating characteristic curve [AUC], 0.89 vs 0.68, respectively).
Personalized Screening Recommendations
The combination of AI systems for short- and long-term breast cancer risk results in improved cancer risk assessment . Diagnostic AI models, trained to detect suspicious lesions on mammograms, are well-suited for estimating short-term breast cancer risk. Texture AI models, capable of identifying breast density, are more suitable for long-term breast cancer risk assessment.
A study published in Radiology showed that a combined AI model, integrating both diagnostic and texture models, demonstrated overall improved risk assessment for both interval and long-term cancer detection.Women identified by the combined model as having the 10% highest combined risk accounted for 44.1% of interval cancers and 33.7% of long-term cancers.
Long-term Patient Monitoring
AI-based predictive analytics monitoring presents a new paradigm of care. Its continuous nature can lead to very early diagnosis and brings the opportunity to be proactive—taking steps toward diagnosis and treatment prior to severe symptoms . Some potentially catastrophic illnesses have prodromal signatures that can be detected by algorithms analyzing continuous cardiorespiratory monitoring
A continuous predictive analytics monitoring system, such as the CoMET monitor, assigns a comet-like icon to each patient in a clinical care unit, displaying the fold-increase in risk from 1 to 5 of a future critical event. This visual representation allows the interprofessional team to easily monitor each patient’s risk, facilitating timely interventions and personalized care strategies.
Conclusion
The integration of AI in radiology is revolutionizing the field, marking a significant shift in how medical imaging is approached and utilized. By enhancing image analysis, automating workflows, and facilitating the fusion of various imaging techniques, AI is fundamentally transforming patient care and diagnostic accuracy. As we move forward, the potential of AI to provide predictive insights and personalized treatment options presents exciting opportunities for both patients and healthcare professionals.
However, it is essential to acknowledge the challenges that accompany these advancements, including ethical considerations and the need for robust validation. By proactively addressing these issues and embracing the innovations AI offers, the radiology community can unlock new levels of efficiency and effectiveness in patient care. Ultimately, the future of radiology, enriched by AI, promises not only to improve diagnostic capabilities but also to redefine the standards of healthcare delivery for generations to come.
FAQs
What are the advantages of using AI in the medical sector?
AI improves the patient experience by enabling digital communication tools that provide appointment reminders, personalized health advice, and recommendations for future steps. Additionally, AI’s role in diagnosing health issues enhances the speed and accuracy of patient visits, offering quicker and more tailored medical care.
How does AI benefit radiotherapy?
AI revolutionizes radiotherapy by improving the segmentation of tumors and organs at risk, significantly reducing the time radiation oncologists need to spend on these tasks. It also plays a crucial role in treatment planning and optimization, cutting down the planning time from days to mere minutes or seconds.
References
[1] – https://www.gehealthcare.com/insights/article/deep-learning-image-reconstruction-improving-iq-and-patient-outcomes-in-radiology https://www.gehealthcare.com/insights/article/deep-learning-image-reconstruction-improving-iq-and-patient-outcomes-in-radiology[2] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10546449/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10546449/
[3] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9328044/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9328044/
[4] – https://www.carestream.com/blog/2021/05/11/smart-noise-cancelation-a-groundbreaking-advance-in-x-ray-image-quality/ https://www.carestream.com/blog/2021/05/11/smart-noise-cancelation-a-groundbreaking-advance-in-x-ray-image-quality/
[5] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10535385/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10535385/
[6] – https://pubs.rsna.org/doi/full/10.1148/rg.2021200113 https://pubs.rsna.org/doi/full/10.1148/rg.2021200113
[7] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8980942/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8980942/
[8] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10487271/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10487271/
[9] – https://www.nature.com/articles/s41598-024-63824-z https://www.nature.com/articles/s41598-024-63824-z
[10] – https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01533-7 https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-021-01533-7
[11] – https://insightsimaging.springeropen.com/articles/10.1186/s13244-024-01660-5 https://insightsimaging.springeropen.com/articles/10.1186/s13244-024-01660-5
[12] – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8458037/ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8458037/
[13] – https://pubs.rsna.org/doi/10.1148/radiol.231849 https://pubs.rsna.org/doi/10.1148/radiol.231849
[14] – https://www.rsna.org/news/2023/august/models-improve-breast-cancer-risk-assessment https://www.rsna.org/news/2023/august/models-improve-breast-cancer-risk-assessment


Add a Comment